Speaker Mike Johnson’s Medicaid cuts threaten healthcare access for thousands in Louisiana.
Overview of Medicaid Cuts
In August 2025, Speaker Mike Johnson proposed reductions to Medicaid funding, a move that immediately raised alarms among healthcare providers and constituents across Louisiana. The plan could affect thousands of residents by narrowing eligibility, tightening benefits, or reducing payments to providers. Any of those steps would weaken the safety net that rural hospitals and community clinics depend on to keep their doors open. Health centers are already drafting contingency budgets because they rely on Medicaid reimbursements to operate day to day. If enacted, the Medicaid cuts would ripple through every level of the state’s health system.
Why Medicaid Matters in Louisiana
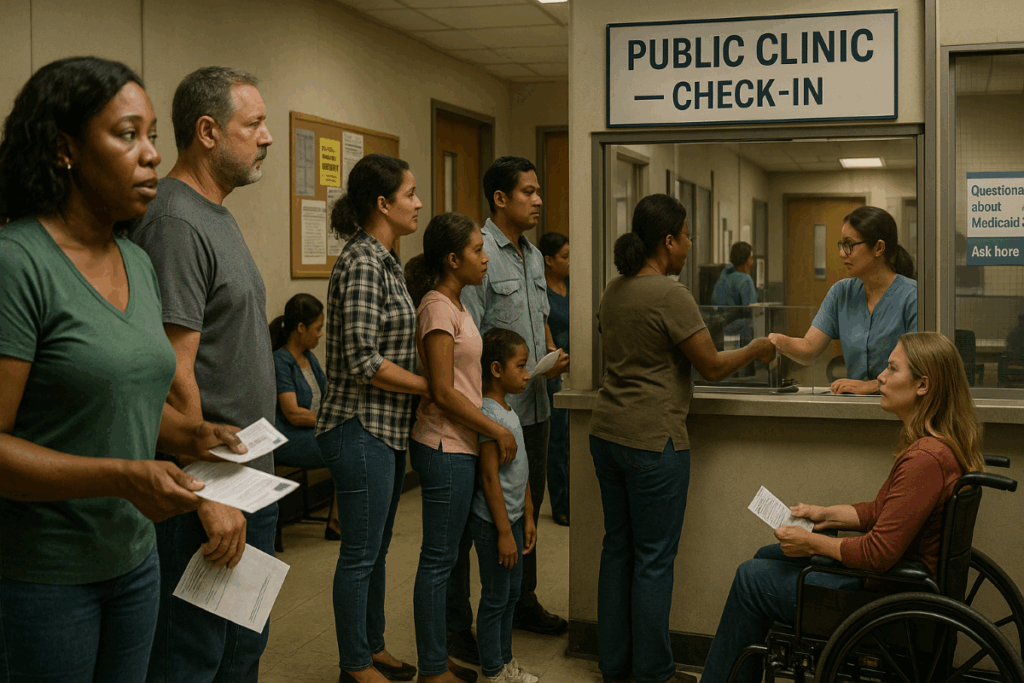
Medicaid is the backbone of care for roughly one in three Louisiana residents, including children, low-income adults, seniors in long-term care, and people with disabilities. It supports primary care, prenatal and postpartum services, mental-health counseling, and prescription drugs. Medicaid also underpins rural hospitals and safety-net clinics that operate on slim margins. When lawmakers pursue Medicaid cuts, the effects travel from clinic waiting rooms to hospital ERs and nursing homes. The program’s dollars keep local providers solvent and ensure that chronic conditions are managed before they become expensive emergencies.
Consequences for Health Centers
Health centers—Federally Qualified Health Centers (FQHCs), parish clinics, and nonprofit primary-care sites—serve as the first and sometimes only point of contact for low-income residents. Many are already operating on thin margins. A decrease in reimbursements can mean immediate service reductions, hiring freezes, or, in worst cases, closures. Leaders at these centers describe contingency plans that include delaying equipment purchases, reducing evening hours, and shrinking outreach programs that help patients navigate insurance and specialty referrals. If Medicaid cuts take effect, clinics will have fewer resources to coordinate care, resulting in sicker patients and higher downstream costs.
Community health clinics that provide screenings, vaccines, lab work, dental care, and referrals are particularly vulnerable. With revenue falling, clinics may be forced to shorten appointment times or reduce the number of new patients they accept each week. Programs launched during the pandemic—mobile vans, telehealth, blood-pressure clubs—could be scaled back even though they have proven effective at catching problems early. The result of broad Medicaid cuts would be fewer touchpoints for preventive care and a rising burden of uncompensated services.
Pressure on Hospitals and Emergency Rooms
Hospitals—especially in rural Louisiana—rely on Medicaid to keep essential services staffed. When coverage shrinks, uncompensated care rises. Patients delay treatment, conditions worsen, and emergency departments shoulder crises that could have been managed in community settings. Louisiana has already lost several labor-and-delivery units over the last decade as volumes fell and budgets tightened. Further financial stress could accelerate closures of obstetrics, psychiatric, and detox beds—precisely the services that stabilize communities. Hospital administrators warn that broad Medicaid cuts would likely trigger hiring freezes, longer wait times, and more transfers out of parish hospitals to already crowded regional centers.
Impact on Patients and Families
Thousands of residents use Medicaid for chronic-condition management—diabetes, hypertension, asthma, heart disease, and serious mental illness. Losing coverage interrupts medication regimens and scheduled check-ins, which leads to preventable complications and costly hospitalizations. Families will also feel the financial strain: without coverage, routine pediatric visits, prenatal care, physical therapy, and durable medical equipment become unaffordable. In a state where many households already juggle rent, utilities, and food costs, Medicaid cuts translate directly into tough choices about whether to seek care at all.
Rural and Vulnerable Communities
The proposed changes risk widening long-standing health disparities. Rural parishes often have fewer providers and longer distances to care. If clinics cut hours or close, people may spend hours on the road or forgo care entirely. Communities of color and people with disabilities—who already face structural barriers—would bear a disproportionate share of the harm. Transportation assistance, community-health workers, and language-access services are frequently financed through Medicaid. When budgets shrink because of Medicaid cuts, these supports often disappear first, even though they deliver outsized benefits for access and outcomes.
Behavioral Health and the Opioid Crisis
Behavioral-health providers depend on Medicaid for counseling, psychiatric visits, and substance-use treatment. If reimbursements fall or eligibility narrows, fewer clinicians will accept Medicaid and waiting lists will lengthen. For people managing depression, PTSD, or opioid-use disorder, treatment interruptions can be life-threatening. Louisiana’s fight against overdose deaths requires consistent care, medication-assisted treatment, and crisis stabilization—services that become harder to sustain when Medicaid cuts undercut reliable funding.
Women’s and Children’s Health
Medicaid pays for a large share of births in Louisiana and ensures well-child visits, immunizations, and developmental screenings. Reduced benefits or tougher eligibility rules would mean missed prenatal appointments, late detection of pregnancy complications, and lower vaccination rates. Over time, that translates into higher infant mortality and more children starting school with untreated health needs. The short-term savings from Medicaid cuts are quickly offset by long-term costs borne by families, schools, and hospitals.
Economic Ripples
Health care is one of Louisiana’s largest employers. Dollars lost through Medicaid are dollars not spent on nurses, lab techs, community-health workers, and local suppliers. When clinics scale back, surrounding businesses—from pharmacies to transportation services—feel the blow. The economic multiplier runs in reverse in small towns when Medicaid cuts drain revenue from the local health system. Job losses and reduced purchasing power ripple through main streets and parish budgets, making it even harder to recruit clinicians or maintain ambulance coverage.
What Patients Can Do Now
Patients worried about losing coverage should verify their contact information with the state, respond promptly to renewal notices, and seek assistance from navigators or health centers if paperwork is confusing. Keep documentation of income, household size, and residency up to date to prevent avoidable disenrollments. If eligibility changes, explore options through the federal marketplace—some families qualify for subsidized plans—or check whether disability, pregnancy, or medically-needy pathways apply. Community clinics can help patients appeal eligibility decisions and connect them with prescription-assistance programs during any transition tied to Medicaid cuts.
Policy Options Under Debate
Critics argue that there are smarter ways to control costs without sacrificing coverage. Options include value-based payment models that reward outcomes, targeted anti-fraud technology, stronger care coordination for high-need patients, and federal waivers that let states innovate while protecting access. Louisiana leaders from both parties have floated measures to streamline administrative processes and improve data-sharing so that care is more efficient. These approaches require planning and accountability, but they avoid the blunt harm caused by across-the-board Medicaid cuts.
Political and Community Response
The political response is divided. Some lawmakers frame reductions as fiscal discipline; others warn of dire consequences for public health, hospitals, and schools that depend on stable community care. Health systems, parish officials, faith organizations, and patient advocates are coordinating outreach, urging legislators to pursue alternatives that preserve coverage. Community groups are organizing listening sessions, petition drives, and town halls to ensure the human stakes of Medicaid cuts remain visible and urgent.
Bottom Line
The reductions under consideration pose a serious threat to access and equity in Louisiana’s health system. Experience from past downturns is clear: when states enact Medicaid cuts, coverage drops, hospitals shoulder more uncompensated care, and outcomes worsen—especially in rural and underserved communities. Protecting coverage now will cost far less than trying to rebuild a shattered safety net later. Louisiana’s path forward should focus on smarter spending, not fewer patients.
Glossary
-
Eligibility redetermination: The yearly process where the state confirms whether a person still meets income and household requirements for Medicaid.
-
Uncompensated care: Hospital or clinic care for which no payment is received from patients or insurers, often due to lack of coverage.
-
Value-based payment: A reimbursement approach that rewards quality outcomes and care coordination rather than paying only for the volume of services.
-
Safety-net provider: A clinic or hospital that serves all patients regardless of ability to pay, often funded through a mix of public and private sources.
Further Reading
Connect with the Author
Curious about the inspiration behind The Unmaking of America or want to follow the latest news and insights from J.T. Mercer? Dive deeper and stay connected through the links below—then explore Vera2 for sharp, timely reporting.
About the Author
Discover more about J.T. Mercer’s background, writing journey, and the real-world events that inspired The Unmaking of America. Learn what drives the storytelling and how this trilogy came to life.
[Learn more about J.T. Mercer]
NRP Dispatch Blog
Stay informed with the NRP Dispatch blog, where you’ll find author updates, behind-the-scenes commentary, and thought-provoking articles on current events, democracy, and the writing process.
[Read the NRP Dispatch]
Vera2 — News & Analysis
Looking for the latest reporting, explainers, and investigative pieces? Visit Vera2, North River Publications’ news and analysis hub. Vera2 covers politics, civil society, global affairs, courts, technology, and more—curated with context and built for readers who want clarity over noise.
[Explore Vera2]
Whether you’re interested in the creative process, want to engage with fellow readers, or simply want the latest updates, these resources are the best way to stay in touch with the world of The Unmaking of America—and with the broader news ecosystem at Vera2.
Free Chapter
Begin reading The Unmaking of America today and experience a story that asks: What remains when the rules are gone, and who will stand up when it matters most? Join the Fall of America mailing list below to receive the first chapter of The Unmaking of America for free and stay connected for updates, bonus material, and author news.